End-to-End Insurance Credentialing & Provider Enrollment
Ready to streamline your path to insurance network participation? At BillingNavigator, our comprehensive credentialing and provider enrollment services ensure your practice is accurately and efficiently enrolled with the top insurance payers. We handle every step—from application preparation to follow-ups—so you can focus on delivering care while maximizing your revenue potential.
Let us make credentialing simple, fast, and stress-free, helping you get paid promptly and join the networks that matter most to your practice.



Schedule a Consultation
End-to-End Credentialing : Read-to-Bill in Record Time
Within 24 Hours
Application Submitted
100%
First-Time Approval Rate
100%
Managed Approval Rate
20% Lower
Administrative Costs
Active CAQH/PECOS
Profile Maintains & Audit
Comprehensive Provider Credentialing Services
Join the nation’s leading insurance networks with confidence. At BillingNavigator, we simplify the credentialing and enrollment process so your practice can start delivering care—and receiving timely reimbursements—without administrative delays.
Our end-to-end credentialing workflow ensures that your qualifications, licensure, and compliance documents are accurately verified and submitted to the right payers. Once credentialed, you gain access to steady patient referrals, improved cash flow, and a more efficient revenue cycle.
Being out-of-network, even temporarily, can prevent you from treating insured patients and billing payers for the services you render. Our credentialing experts ensure this never happens to your practice.
Provider Enrollment & Credentialing
Our provider enrollment and credentialing experts streamline the entire approval process with major insurance payers. We collect, verify, and submit all required documents to ensure your credentials are accurately reviewed. From application preparation to status monitoring, we help you secure active provider participation with every payer.
Insurance Credentialing Services
Our insurance credentialing services support all major healthcare plans, including commercial payers, Medicare, and Medicaid. We manage CAQH profiles, application preparation, primary source verification, and payer follow-ups. This ensures accurate, compliant, and timely credentialing so your practice remains in-network without interruptions.
PECOS & CMS/Medicare Credentialing
Our Medicare credentialing team manages PECOS enrollment, revalidation, reassignment of benefits, and Medicare ID setup. We ensure all documents meet CMS standards and guide providers through each step of the enrollment process. This minimizes delays and secures active Medicare participation for your practice.
Payer Contract Management
Our payer contract management service supports negotiations, renewals, and fee schedule reviews with insurance networks. We help providers understand reimbursement terms, identify improvement opportunities, and secure favorable contract conditions. Our goal is to maximize payer revenue while reducing administrative burden.
Clearinghouse Enrollments
We simplify clearinghouse enrollment by managing the full setup for electronic claims, remittances, and eligibility transactions. Our team ensures seamless EDI connectivity with payers, enabling faster claims submission, improved accuracy, and secure end-to-end digital data exchange between providers and payers.
Hospital Credentialing Services
Our insurance credentialing services support all major healthcare plans, including commercial payers, Medicare, and Medicaid. We manage CAQH profiles, application preparation, primary source verification, and payer follow-ups. This ensures accurate, compliant, and timely credentialing so your practice remains in-network without interruptions.
Healthcare Licensing Services
We assist healthcare professionals with new state licenses, renewals, verifications, and license transfers. Our team manages documentation, board requirements, and state-specific compliance guidelines to ensure timely approvals. This helps providers maintain active licensure and uninterrupted eligibility to deliver care.
Re-Credentialing Services
We manage your entire re-credentialing cycle to keep your status active with payers. From updating CAQH and renewing documents to submitting re-credentialing applications and addressing payer requests, we ensure continuous compliance and prevent service interruptions. Stay in-network with zero administrative stress.
Outsource Medical Credentialing Services to Billingnavigator
Considering outsourcing your medical credentialing but unsure about cost, security, or efficiency? At BillingNavigator, we eliminate those concerns with a transparent, streamlined, and fully compliant credentialing experience tailored for healthcare providers.
Outsourcing your credentialing to our expert team significantly reduces paperwork, administrative time, and operational costs. We manage every step—application preparation, documentation, payer follow-ups, CAQH updates, enrollments, and contract execution—so you can focus entirely on patient care.
As your trusted credentialing partner, we maintain direct communication with insurance representatives to accelerate approvals, remove bottlenecks, and ensure you become an in-network provider without delays.
Discover the BillingNavigator Advantage a smarter, faster, and more reliable way to complete your medical credentialing.

Centralized Project Management System
At BillingNavigator, efficiency and transparency guide everything we do. Our credentialing workflow is managed through a secure, centralized project management system designed to streamline communication and track every step of your application. This password-protected platform safeguards your sensitive information while ensuring that all credentialing tasks are completed accurately, efficiently, and on time.
Dedicated Account Manager
Each provider is paired with a dedicated account manager who serves as your single point of contact throughout the credentialing and enrollment process. They offer personalized guidance, handle complex payer requirements, and ensure that your applications move forward without delays. Their commitment ensures clear communication, faster resolutions, and an exceptional client experience.
Cost-Effective Credentialing Solutions
Building and maintaining an in-house credentialing department can be costly—it requires hiring, training, infrastructure, and ongoing administrative resources. With BillingNavigator, you eliminate those overhead expenses. Our outsourced credentialing model provides expert support at a fraction of the cost, allowing your practice to benefit from professional credentialing without the financial burden.
Efficient Provider Registration
CAQH, PECOS, NPPES, and payer databases require ongoing updates to maintain accurate provider profiles. Our credentialing specialists handle all registrations, updates, and maintenance tasks to keep your information current across all platforms. This ensures timely verification by insurance companies and prevents avoidable delays in the credentialing process.
Bi-Weekly Credentialing Status Updates
To maintain full transparency, your account manager provides bi-weekly updates on the progress of every credentialing application. They track statuses, follow up with payers, and maintain detailed reports that can be sent to you anytime. These updates help you stay informed, make timely decisions, and maintain confidence in the credentialing process.
Our Medical Insurance Credentialing Process
Every stage of our medical insurance credentialing process is carefully structured to accelerate approvals and keep your applications moving efficiently—typically within 120 days. Through rigorous verification, regulatory compliance checks, and thorough licensure reviews, we eliminate delays and ensure a smooth credentialing experience that supports your practice’s financial success.
1. CAQH Profile Review & Setup
We begin by reviewing your existing CAQH profile to ensure all credentials and data are current. If updates are required, we make them immediately. For providers without a CAQH account, we create a complete profile on CAQH ProView to initiate the credentialing process without delays.
2. Data & Document Collection
We prepare a consolidated enrollment file containing all required documents. Your information is uploaded to our secure, password-protected system, which follows strict HIPAA compliance standards. This ensures your credentials remain accurate, protected, and ready for payer submission.
3. Project Management & Tracking
Each provider receives a dedicated credentialing project in our management system. This allows us to assign tasks, track progress, and maintain seamless communication. The platform acts as a centralized hub for updates, ensuring transparency at every stage.
4. Application Submission
Once all documents are verified, we submit complete, error-free applications to the targeted insurance payers. Our goal is to start the credentialing process immediately by ensuring each application is accurate and aligned with payer requirements.
5. Follow-Ups & Payer Communication
We actively monitor all applications and maintain continuous follow-up with insurance representatives. Our team provides regular updates, resolves payer requests, and ensures your credentialing moves forward without unnecessary waiting periods.
6. Contracting & Effective Date Setup
After approval, we assist with contract signing, fee schedule review, and effective date confirmation. A copy of your payer agreements is stored securely within our portal for 24/7 access. We also support reimbursement rate negotiations when requested.
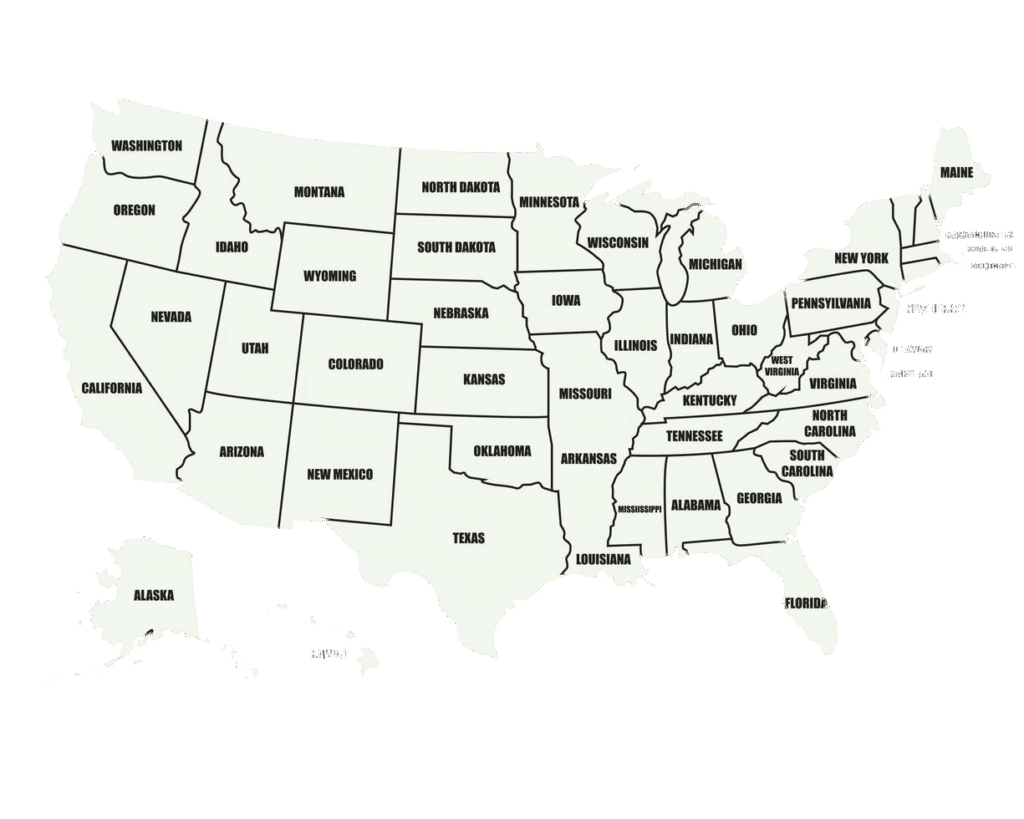
We Are Available Nationwide
Get your claims approved the first time! At BillingNavigator, our team consistently achieves a 95% first-pass clean claims rate. We identify and eliminate claim errors before submission, ensuring faster approvals and maximum reimbursements. Our proven process helps providers reduce rework, minimize denials, and maintain a smooth revenue cycle.
Schedule a Consultation
24/7 Support Across All Specialties
At BillingNavigator, we provide around-the-clock credentialing support for healthcare providers across every specialty—from nephrology and neurology to cardiology, dermatology, and beyond. Our credentialing specialists are trained in the specific payer requirements for each discipline, ensuring accurate guidance and a streamlined enrollment process.
No matter your location or time zone, our team is available 24/7 to answer questions, resolve issues, and keep your credentialing applications moving without delays. With BillingNavigator, expert support is always within reach.
Cardiology
Gastroenterology
Oncology
OBGYN
Anesthesia
Neurology
Orthopedic
Radiology
Pediatric
Urology
Lowest Prices Guaranteed
Looking for expert medical credentialing support without exceeding your budget? At BillingNavigator, we offer high-quality provider enrollment and insurance credentialing services at competitive, affordable rates. Our goal is to make credentialing accessible to healthcare providers across the U.S. while maintaining the highest standards of accuracy, compliance, and efficiency.
Get in Touch with a Medical Credentialing Specialist
Have questions about our credentialing services or need guidance on where to begin? Connect with BillingNavigator today. Our credentialing specialists will evaluate your practice’s needs and provide a customized solution designed to simplify your enrollment process, reduce delays, and help you become an approved in-network provider with confidence.

FAQs
What is Primary Source Verification (PSV)?
Primary Source Verification is the process through which insurance payers or healthcare facilities directly verify a provider’s education, training, certifications, and other qualifications from the original issuing source. PSV strengthens patient safety, ensures the provider is competent, and protects organizations against negligent credentialing risks.
What is provider enrollment and credentialing?
Credentialing verifies a provider’s qualifications, training, and clinical competence.
Enrollment is the next step—where the provider joins an insurance network and becomes eligible to bill that payer. Both processes work together to establish complete in-network status.
Can a non-credentialed provider see patients?
Sometimes. A provider may see patients under supervision while credentialing is in progress, depending on payer and facility policies. However, independent patient care without credentialing is not recommended.
Are physicians re-credentialed yearly?
Typically, physicians must complete re-credentialing every 1–3 years, depending on the insurance payer or facility requirements.
Can physicians complete Medicare credentialing before receiving a DEA license?
Yes—if the provider does not prescribe or administer controlled substances. In such cases, the DEA field on the application can be marked “Not Applicable.” However, obtaining a DEA license is recommended for broader practice eligibility.
What is insurance credentialing?
Insurance credentialing is the process where payers review and verify a healthcare provider’s qualifications to determine eligibility for joining their network. It is the first step in enabling a provider to bill insurance companies for patient care.
What are status codes in healthcare coding?
HCPCS status codes defined by CMS indicate whether a code is payable separately, bundled into another service, or not reimbursable under Medicare.
What documents do I need to start credentialing?
Commonly required documents include your medical license, DEA certificate, malpractice insurance, CV, board certifications, W-9, NPI, education history, and any state-specific documents. We provide a complete checklist to ensure nothing is missed.
What is the difference between credentialing and contracting?
Credentialing verifies your qualifications; contracting establishes your reimbursement rates and the terms under which you join the payer network. BillingNavigator manages both from start to finish.
Can BillingNavigator help with Medicare PECOS enrollment?
Absolutely. We handle PECOS setup, reassignments, revalidations, and Medicare enrollment to ensure full compliance and timely approval.
Do I need credentialing if I’m an independent contractor?
Yes. Independent providers must be credentialed to bill payers, unless they exclusively work under another provider’s supervision following incident-to rules.
Can credentialing affect my reimbursement rates?
Yes. Proper credentialing and contracting ensure you receive accurate payer reimbursement according to your negotiated fee schedule.
What if my credentialing expires?
Yes. Whether you practice telehealth or operate in multiple states, we manage licensing, payer enrollment, and credentialing across all required jurisdictions.
Why is credentialing important for medical assistants?
Credentialing confirms a medical assistant’s skills, knowledge, and competency, making them legally eligible to practice. It strengthens professional credibility and supports long-term career growth.
Can a non-credentialed provider bill under another provider?
In certain cases, yes. A new provider may bill under a supervising provider’s NPI if the insurance payer allows incident-to billing and if the practice meets all eligibility requirements. Always verify the payer’s rules before proceeding.
What is the credentialing process for physicians?
Physician credentialing includes verification of education, training, licenses, work history, malpractice coverage, certifications, and professional performance to ensure the provider is qualified to deliver patient care.
Can non-credentialed physicians bill Medicare?
No. Providers must be fully credentialed and enrolled with Medicare before billing for services.
What is hospital credentialing?
Hospital credentialing verifies a provider’s qualifications, clinical experience, and competency before granting privileges to practice within a hospital setting.
How do I get credentialed with insurance companies?
To credential with a payer, you must:
- Review their requirements
- Complete the application
- Submit all supporting documents
- Provide any additional information requested
- Follow up consistently until approval
BillingNavigator can manage all these steps for you.
How long does the credentialing process usually take?
Credentialing with insurance payers typically takes 90–120 days, depending on the payer, document accuracy, and response times. BillingNavigator helps expedite the process through proactive follow-ups and complete, error-free submissions.
Can BillingNavigator manage my CAQH profile?
Yes. We create, update, and maintain your CAQH ProView profile, ensuring all information, attestations, and documents remain current for payer access during credentialing.
Do I need to be credentialed separately for each insurance company?
Yes. Each payer requires its own application, documentation, and approval. Our specialists manage submissions and follow-ups across all major commercial, Medicare, and Medicaid plans.
What happens if my application is denied?
If a payer denies your application, we identify the cause, correct any discrepancies, submit appeals when applicable, and resubmit to ensure approval.
Do group practices need separate credentialing?
Yes. Both the group and the individual providers must be credentialed and enrolled. BillingNavigator manages both entity and individual applications.
How do I keep my credentials active?
Providers must keep CAQH, medical licenses, malpractice certificates, and all payer information up to date. BillingNavigator monitors expirations and manages re-credentialing to prevent interruptions.
Do you handle multi-state credentialing?
Providers must keep CAQH, medical licenses, malpractice certificates, and all payer information up to date. BillingNavigator monitors expirations and manages re-credentialing to prevent interruptions.
Can I start seeing patients before I’m credentialed?
Some payers allow supervised visits or “credentialing in process,” but many do not. BillingNavigator provides guidance based on your payer mix to avoid compliance issues.

