Payment Posting
Payment Posting Services
Ensure Total Accuracy. Strengthen Your Revenue Cycle.
At BillingNavigator, we understand that accurate payment posting is the backbone of a healthy revenue cycle. Our team meticulously records all insurance and patient payments, verifies posting accuracy, identifies discrepancies, and flags underpayments—so every dollar is captured, reconciled, and accounted for.
With our fully streamlined process, your practice can stay focused on patient care while we handle the administrative workload with precision and reliability.
Schedule a Consultation
Why Choose BillingNavigator for Payment Posting?
- Accurate Payment Allocation
Every payment is carefully posted to the correct patient account, visit, and CPT code. - Quick Identification of Errors & Underpayments
We detect variances, incorrect adjustments, and missing payments before they impact your revenue. - Clean, Organized Financial Records
Clear and accurate posting ensures smooth reconciliation and reduces billing follow-up work. - Reduced Administrative Burden
Free up your staff from time-consuming manual tasks. - Improved Cash Flow
Faster, accurate posting supports timely financial reporting and efficient revenue cycle operations.



Optimize RCM with Expert Payment Posting Services
< 30
Days in AR
10-15%
Revenue Increase
97%
First Pass Ratio
96%
Collection Ratios
98%
Clean Claims Rate
What Is Payment Posting Services in Healthcare
Claim denials are among the most common challenges affecting the financial stability of healthcare organizations across the United States. Each year, hospitals spend over $20 billion managing denials, with an average of $5 million in annual write-offs due to unresolved claims. These issues not only disrupt revenue flow but also increase administrative burdens and lower staff productivity.
Handling denials in-house can be costly and time-consuming. Without specialized expertise, healthcare providers often face delays in identifying root causes, correcting claim errors, and managing appeals efficiently.
At BillingNavigator, we provide comprehensive Denial Management Services tailored to your organization’s unique needs. Our experienced team analyzes denial trends, corrects errors at their source, and implements effective strategies to prevent future rejections. We manage the entire process—from root-cause analysis to appeals—ensuring faster reimbursements and improved cash flow.
Partner with BillingNavigator to reduce denial rates, recover lost revenue, and strengthen your revenue cycle management. Focus on delivering quality patient care while we handle the complexities of denial management with accuracy and expertise.
Why Payment Posting Matters
A strong payment posting workflow ensures:
- Real-time insight into your financial performance
- Accurate patient balances after posting copayments, deductibles, and coinsurance
- Immediate identification of underpayments or discrepancies
- Faster denial detection and correction
- Clean and organized patient accounts
- Improved cash flow and streamlined claim management
Payment posting can be performed manually or through automated systems, but for consistent accuracy and efficiency, many practices choose to outsource payment posting to BillingNavigator.
Types of Payment Posting Services We Offer
At BillingNavigator, we ensure that every payment—down to the last cent—is posted accurately and efficiently. Our comprehensive payment posting solutions enhance transparency across your revenue cycle and strengthen your financial performance. From processing Electronic Remittance Advice (ERA) files to managing denials and patient responsibility, our team is equipped to handle all aspects of your payment posting needs.
Electronic Remittance Advice (ERA) Posting
Automated and accurate posting of ERA files to ensure clean, timely entries.
Manual EOB Payment
Posting
Careful posting of Explanation of Benefits (EOBs) when electronic files are unavailable.
Copayment, Deductible & Coinsurance Posting
Precise allocation of patient-responsibility amounts for complete account accuracy.
Insurance Payment Posting
Recording payments, adjustments, and write-offs from all major insurance payers.
Patient Payment Posting
Efficient posting of cash, credit card, and check payments collected at the time of service or afterward.
Denial & Partial Payment Identification
Immediate flagging of denials, variances, and underpayments for quick follow-up.
Secondary & Tertiary Balance Transfer
Ensuring correct movement of remaining balances to secondary or tertiary payers.
Payment Reconciliation & Reporting
Clear, organized reconciliation summaries to keep your financial records fully aligned.
Our Payment Posting Process
At BillingNavigator, we understand that accurate payment posting is essential to maintaining the financial stability of your practice. That’s why we follow a structured, detail-oriented workflow designed to improve accuracy, enhance visibility, and strengthen your overall revenue cycle. Our systematic approach ensures that every payment is captured, verified, and reconciled supporting cleaner claims, faster reimbursements, and improved revenue performance.
1. Data Collection
We start our payment posting process with data collection. We conduct several meetings with our clients to gather all relevant payment information, including all Electronic Remittance Advice (ERA) and Explanation of Benefits (EOBs) they received from the payers.
2. Verification
The next step after data collection is verification. Our team verifies all the gathered information and makes sure that your payments are complete and align perfectly with the services provided through multiple checklists.
1. Data Collection
We start our payment posting process with data collection. We conduct several meetings with our clients to gather all relevant payment information, including all Electronic Remittance Advice (ERA) and Explanation of Benefits (EOBs) they received from the payers.
1. Data Collection
We start our payment posting process with data collection. We conduct several meetings with our clients to gather all relevant payment information, including all Electronic Remittance Advice (ERA) and Explanation of Benefits (EOBs) they received from the payers.
Why Outsource Payment Posting to Billingnavigator
At BillingNavigator, we understand that accurate payment posting is essential to maintaining the financial stability of your practice. That’s why we follow a structured, detail-oriented workflow designed to improve accuracy, enhance visibility, and strengthen your overall revenue cycle. Our systematic approach ensures that every payment is captured, verified, and reconciled supporting cleaner claims, faster reimbursements, and improved revenue performance.
Proactive Error Detection
Stay ahead of issues. Our specialists identify discrepancies, underpayments, and denials early—helping you recover revenue faster.
Proactive Error Detection
Stay ahead of issues. Our specialists identify discrepancies, underpayments, and denials early—helping you recover revenue faster.
Customized Posting Solutions
Get services tailored to your practice. Whether you handle high-volume claims or specialty-specific billing, we adapt to your unique needs.
Dedicated Support Team
Support you can count on. Our experts are always available to answer questions, resolve issues, and keep your revenue cycle running smoothly.
Unmatched Accuracy
Experience flawless payment posting with BillingNavigator. Our team records every detail with precision, reducing errors and ensuring your revenue is tracked accurately and consistently.
Advanced Security Measures
Your financial data is always protected. BillingNavigator uses advanced security systems and routine audits to safeguard sensitive information and maintain the highest level of data integrity.
HIPAA-Compliant Payment Posting
We prioritize confidentiality and compliance. All BillingNavigator services fully meet HIPAA standards, ensuring your patients’ health information remains secure and protected.
Industry Expertise & Continuous Training
Benefit from a highly skilled team. Our experienced payment posting specialists understand payer rules, adjustments, and complex billing scenarios—and receive ongoing training to maintain exceptional accuracy.
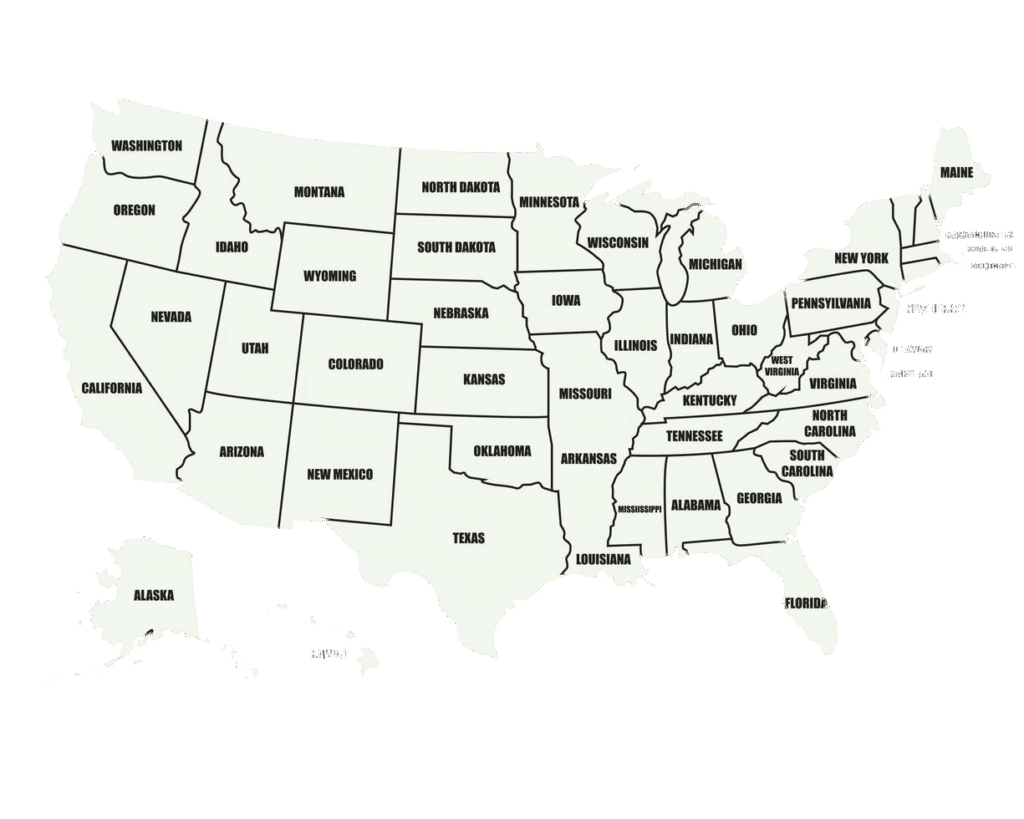
We Are Available Nationwide
Get your claims approved the first time! At BillingNavigator, our team consistently achieves a 95% first-pass clean claims rate. We identify and eliminate claim errors before submission, ensuring faster approvals and maximum reimbursements. Our proven process helps providers reduce rework, minimize denials, and maintain a smooth revenue cycle.
Schedule a Consultation
24/7 Support Across All Specialties
Get reliable assistance whenever you need it. BillingNavigator provides round-the-clock support for all medical specialties—ensuring your payment posting and billing operations run smoothly at all times.
Cardiology
Gastroenterology
Oncology
OBGYN
Anesthesia
Neurology
Orthopedic
Radiology
Pediatric
Urology
Lowest Prices Guaranteed
BillingNavigator delivers high-quality payment posting at the most competitive rates. Get accurate, reliable results while staying well within your budget.
Get in Touch with a Payment Posting Specialist
Have questions or need support? Connect with a BillingNavigator payment posting specialist today. Our experts are ready to streamline your workflow, reduce errors, and strengthen your revenue cycle.

FAQs
What does a payment posting specialist do?
A payment posting specialist records and reconciles all insurance and patient payments, ensures correct allocations, and identifies any discrepancies to maintain accurate patient accounts.
What is the first step in posting a payment?
The first step is verifying the patient’s account information to ensure all payment details and balances are accurate before posting.
What is the difference between cash posting and payment posting?
Cash posting focuses on payments made directly by patients, while payment posting includes all payment types—insurance, patient, checks, credit cards, and more.
What is manual posting in medical billing?
Manual posting is when staff enter payment details by hand or keyboard, often used for cash, checks, or information not captured electronically.
What is auto-posting in medical billing?
Auto-posting uses billing software to record payments automatically—speeding up the process and reducing manual entry errors.
What is an ERA in payment posting?
An Electronic Remittance Advice (ERA) is the digital version of an EOB that allows faster, automated payment posting directly into your billing system.
What is charge posting?
Charge posting is the process of entering CPT-based service charges, including procedure codes, diagnoses, and dates of service, into the billing system.
What is the difference between an EOB and an ERA?
An EOB is a paper statement mailed by insurers, while an ERA is an electronic statement sent through secure digital channels for automated posting.
Why is it important to post charges, payments, and adjustments promptly?
Timely posting helps prevent delays, supports accurate cash-flow tracking, and ensures outstanding balances are identified and managed quickly.
Why is payment posting an important part of RCM?
Payment posting strengthens the revenue cycle by improving cash flow, identifying payment errors early, and ensuring accurate financial reporting.

