Charge Entry
Expert Charge Entry Management Services
Ensure your practice receives every dollar it deserves with BillingNavigator’s precise and compliant Charge Entry Services. Our team carefully captures all patient and service details, verifies coding accuracy, and posts charges promptly to maintain a steady and predictable revenue cycle.
By enhancing billing accuracy through thorough data entry, correct CPT/ICD/HCPCS code reporting, and timely charge posting, we help your practice reduce claim errors, prevent denials, and accelerate reimbursements.



Schedule a Consultation
Certified Charge Entry Specialist
< 30
Days in AR
10-15%
Revenue Increase
97%
First Pass Ratio
96%
Collection Ratios
98%
Clean Claims Rate
What Is Charge Entry in Medical Billing?
Charge entry is a critical step in the medical billing cycle, ensuring that every billable service delivered to a patient is accurately recorded and entered into the billing system. This process directly impacts clean claim submission, timely reimbursements, and the overall financial health of your practice.
At BillingNavigator, our Charge Entry process goes beyond basic data entry. Each encounter is carefully reviewed to verify patient information, provider details, service dates, units, and documentation accuracy. We also ensure that appropriate CPT, HCPCS, and ICD-10 codes are assigned based on standardized medical coding guidelines.
Precise charge entry supports the creation of complete, compliant, and error-free claims reducing denials and maximizing revenue collection. With meticulous attention to detail, our specialists help your practice maintain accuracy, prevent billing mistakes, and optimize reimbursement outcomes.
Medical Charge Charge Entry Services We Offer
A precise and efficient charge entry process is essential for determining the correct reimbursement your practice receives from insurance payers. At BillingNavigator, we provide a comprehensive suite of charge entry services designed to enhance accuracy, strengthen claim quality, and improve your overall revenue cycle.
Our end-to-end charge entry workflow includes every critical sub-process—from charge capture to charge scrubbing—ensuring that all patient, provider, and service details are accurately recorded and compliant with payer requirements. By eliminating errors at the entry level, we help your practice submit clean claims, reduce denials, and accelerate payment turnaround.
Charge Capture
We accurately capture all billable services provided to patients by reviewing clinical documentation, encounter notes, and electronic health records (EHR). Our process ensures every charge is recorded in real time and aligned with payer-specific requirements—preventing missed charges and supporting consistent revenue growth.
Patient Verification
We thoroughly review patient demographics, insurance details, coverage limits, and benefits before charge entry. By verifying this information upfront, we help your practice avoid denials related to incorrect or outdated data—ensuring clean claims and faster reimbursements.
Quality Checks
Before submission, each charge undergoes multiple quality checks to confirm accuracy, completeness, and compliance with payer rules. Our QA process identifies documentation gaps, coding inconsistencies, and data issues—ensuring error-free claims and protecting your practice from costly rework.
New Account Creation
When a new patient visit occurs, we create and verify the patient’s account with complete demographic, insurance, and eligibility details. This ensures that all future charges flow smoothly through the billing system. Accurate account creation helps eliminate rejections, accelerates claim approval, and ensures payments are posted without delay.
Medical Coding
Our coding specialists review provider notes to ensure the correct ICD-10, CPT, and HCPCS codes are applied for each diagnosis, procedure, and service. Proper coding not only reduces denials but also ensures your practice receives the maximum allowable reimbursement for every encounter.
Charge Scrubbing
Every charge is reviewed through advanced charge scrubbing to detect missing modifiers, incorrect codes, inconsistent units, or payer-specific issues. By resolving these errors before claims are submitted, we significantly improve first-pass acceptance rates and strengthen your overall RCM performance.
The BillingNavigator Charge Entry Workflow
The primary goal of an efficient charge entry process is to accurately determine the reimbursement your practice is entitled to for the services provided. At the completion of this process, all verified charges—along with the total compensation expected from the insurance payer—are precisely entered into your billing system. This ensures clean claim creation, timely submission, and a smoother revenue cycle for your practice.
1. Reviewing Medical Records
The process begins with a careful review of the provider’s medical records, such as EHR and EMR systems. During this step, the specialist identifies all billable services provided to the patient and confirms the supporting documentation. This ensures that accurate medical codes and charges are assigned and helps verify that services are captured correctly for optimal reimbursement.
2. Entering Patient Information
Next, the data entry specialist records the patient’s complete information into the billing system under their designated account. This includes demographic details, insurance information, provider data, and services rendered during the visit. Outdated or incomplete data is updated at this stage to ensure a clean and accurate encounter record.
3. Assigning Medical Codes
Using standardized coding systems such as ICD-10, CPT, and HCPCS, the coding specialist assigns appropriate codes for each diagnosis, procedure, and service. Accurate coding makes it easier for payers to understand what was done and why, supporting faster, more precise claim processing and appropriate reimbursement.
4. Computing Total Fees
Charges are then entered or calculated for each service based on the practice’s fee schedule and the assigned medical codes. If a fee schedule is available, the system automatically pulls the correct amounts. Otherwise, the specialist manually inputs the charges. This step ensures that every billable service is translated into the correct dollar value.
5. Reviewing Entered Information
Before the claim is submitted, a final quality check is performed. The charge entry expert (or automated charge scrubber) reviews all patient details, codes, and fees to spot any errors, omissions, or inconsistencies. Any issues are corrected at this stage to reduce denials and delays in the revenue cycle.
6. Submitting Charges
In the final step, the completed claim is transmitted to the billing team or directly to the payer. Once submitted, the provider can track the claim through the revenue cycle and monitor reimbursement. A clean, accurate submission at this stage helps ensure timely payment and a smoother financial experience for both provider and patient.
Why Outsource Charge Entry Services to Billingnavigator
Charge entry plays a crucial role in determining how much your practice ultimately gets paid. When performed with accuracy and compliance, it supports clean claim submission, maximizes reimbursements, and strengthens your cash flow. However, when done incorrectly, it can result in underpayments, claim denials, delayed revenue, and costly rework.
By outsourcing your charge entry process to BillingNavigator, you gain access to a team of experienced billing specialists who ensure accuracy at every stage. From verifying complete patient information to applying correct medical codes, calculating precise charges, and performing detailed quality reviews—our experts manage the entire workflow with precision and compliance.
Partnering with BillingNavigator helps eliminate errors, reduce administrative burden, and boost your revenue cycle efficiency. Let our charge entry professionals handle the complexities so your practice can stay focused on delivering quality patient care.
Accurate Charge Entry
At BillingNavigator, accuracy is our priority. Our charge entry specialists are rigorously trained, detail-oriented professionals who verify every patient detail, service entry, and charge calculation with exceptional precision. We ensure that only complete, correct, and compliant data enters your billing system—reducing errors, eliminating discrepancies, and maximizing reimbursement outcomes.
Cost-Effective Solutions
We deliver premium-quality charge entry services at highly competitive rates. Our pricing model is designed to give small and solo practices access to top-tier billing support at a fraction of the market cost. With BillingNavigator, you benefit from expert service without the financial burden—allowing your practice to maintain profitability while improving billing performance.
Secure Data Management
Your data security is our responsibility. BillingNavigator uses a centralized, access-controlled system to store and manage billing information securely. We maintain strict HIPAA compliance and implement advanced security protocols to protect the privacy of your practice and patients. Only authorized billing specialists access the data—ensuring maximum confidentiality and peace of mind.
Medical Coding Expertise
Our charge entry team collaborates closely with AAPC-certified medical coders to ensure coding accuracy at every step. Whether it’s diagnoses, procedures, treatments, or medical equipment, we apply the correct ICD-10, CPT, and HCPCS codes with the highest level of specificity. This ensures cleaner claims, fewer denials, and faster reimbursements for your practice.
Quick Turnaround Time
Speed without compromise—that’s our promise. BillingNavigator specialists work efficiently to capture, verify, and enter charges within the shortest turnaround time. We understand that timely charge entry directly impacts your cash flow. The faster we complete the process, the sooner your claims can be submitted and reimbursed.
Advanced Technology & Automation
Technology drives our efficiency. BillingNavigator integrates modern billing tools and automation systems to streamline charge entry, detect errors in real time, and enhance overall accuracy. Our tech-forward approach helps reduce manual work, minimize delays, and maintain consistent billing performance—keeping your practice ahead in today’s fast-paced healthcare environment.
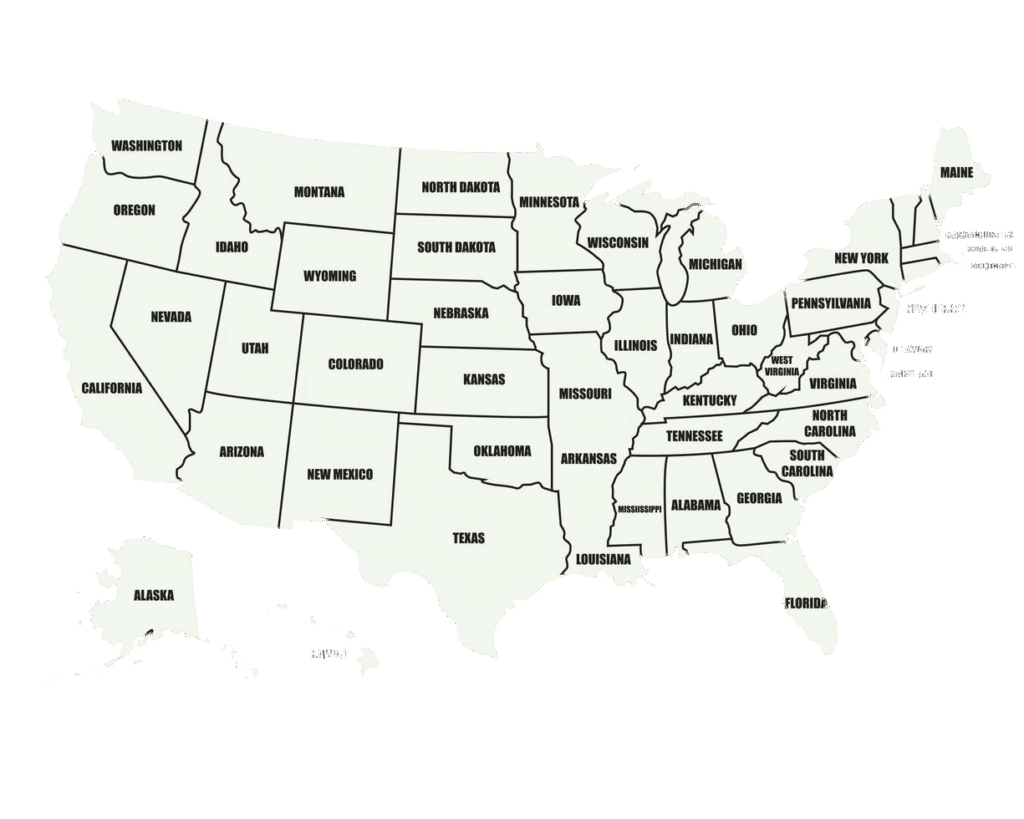
We Are Available Nationwide
Delivering unmatched charge entry expertise nationwide! Our remote operability and virtual setup allow us to provide end-to-end charge entry services in every state and zip code. Our team’s deep understanding of local laws, regulations, and payer policies ensures compliance, preventing legal actions and contract terminations. So, if you need assistance recording accurate charges for the services rendered to your patients, contact us today. We are unrestricted by time and distance!
Schedule a Consultation
24/7 Support Across All Specialties
At BillingNavigator, we provide continuous, round-the-clock support to ensure your practice never faces billing challenges alone. Whether you need help identifying the correct code for a complex procedure or clarifying service fees for specialized tests, our charge entry experts are available 24/7 to guide you.
Our team supports all medical specialties and can be reached anytime via phone, live chat, or email ensuring you receive prompt, accurate, and reliable assistance whenever you need it.
Cardiology
Gastroenterology
Oncology
OBGYN
Anesthesia
Neurology
Orthopedic
Radiology
Pediatric
Urology
Get in Touch with a Charge Entry Specialist
Struggling to keep up with the demands of medical charge entry? BillingNavigator is here to help. Our experienced charge entry specialists accurately input service details, apply the correct medical codes, and calculate precise charges—ensuring your claims are submitted cleanly and reimbursed quickly.
Connect with our team today to streamline your billing process and strengthen your practice’s revenue cycle with reliable, error-free charge entry support.

FAQs
What is an example of charge entry in medical billing?
Charge entry is the step where all the charges for a patient’s visit are entered into the billing system to prepare the claim.
Example:
After a patient’s appointment, the charge entry specialist receives all the finalized codes from the coder (for office visit, lab tests, injections, etc.). The specialist then:
- Enters each code into the billing software
- Confirms the correct units, modifiers, and provider details
- Verifies the patient’s insurance and fee schedule
- Let’s the system calculate the total amount the provider expects to receive from the insurance payer
This is Charge entry in action—turning coded services into a clean, billable claim ready for submission.
What is the difference between charge entry and charge capture?
Both steps are part of the same revenue cycle, but they happen at different times and focus on different tasks.
- Charge capture
- Purpose: Make sure all billable services are identified and not missed.
- What happens: Clinical documentation and EMR notes are reviewed to capture every service performed—for example, office visits, surgical procedures, drug administration, diagnostic tests, and post-operative care.
- Goal: Prevent lost revenue by ensuring no service is left unbilled.
- Charge entry
- Purpose: Convert those captured services into a structured, billable claim.
- What happens: The already captured services (and their codes) are entered into the billing software using CPT, ICD-10, HCPCS, etc.
- Goal: Prepare a clean, accurate claim that payers can process without delays or denials.
In simple terms: charge capture finds the charges, charge entry inputs them into the system for billing.
What is the difference between charge capture and coding?
Charge capture and medical coding work hand-in-hand but focus on different parts of the billing process.
- Charge capture
- Focus: What was done?
- The team reviews physician notes, orders, and EMR documentation to identify all services provided to the patient and match them with the practice’s fee schedule.
- It is often the first step toward creating a complete and clean claim so no service is overlooked.
- Medical coding
- Focus: How do we describe it on the claim?
- Once services and diagnoses are identified, they are translated into standardized codes such as CPT, CDT, HCPCS, and ICD-10.
- These codes tell the payer exactly what was done and why, in a language every insurer understands.
Put simply: charge capture confirms every service that should be billed; coding turns those services and diagnoses into standardized codes so the claim can be paid correctly.

