Healthcare Revenue Cycle Management (RCM)
Healthcare Revenue Cycle
Management (RCM) Services
Optimize your practice’s financial performance with BillingNavigator’s end-to-end RCM solutions. We streamline every step of the revenue cycle—from accurate coding and error-free claim submission to efficient A/R follow-up and transparent reporting—to minimize denials and accelerate reimbursements. Trust our experts to keep your revenue flowing smoothly while you stay focused on patient care.



Schedule a Consultation
Boost Financial Performance with Reliable Revenue Cycle Services
< 30
Days in AR
10-15%
Revenue Increase
97%
First Pass Ratio
96%
Collection Ratios
98%
Clean Claims Rate
Customized Healthcare RCM Services for Your Practice
Finding the right RCM solution can be overwhelming. At BillingNavigator, we offer customized revenue cycle management services designed to optimize your practice’s financial performance. Our team of RCM specialists works closely with you to understand your unique needs and deliver a tailored solution that maximizes reimbursements, reduces denials, and improves cash flow—all within your budget. Schedule a call with our experts today and let us streamline your revenue cycle while you focus on patient care.
Revenue Integrity
Maintain accurate documentation, coding, and charge capture while minimizing compliance risks to maximize reimbursements.
Revenue Cycle Analytics
Turn data into actionable insights with comprehensive reporting that helps you optimize revenue performance.
RCM for Physicians
Comprehensive services including denial management, A/R follow-up, and payment reconciliation for reliable physician revenue.
Reimbursement Management
Maintain accurate documentation, coding, and charge capture while minimizing compliance risks to maximize reimbursements.
RCM for Hospitals
Specialized RCM solutions to improve efficiency, reduce denials, and protect margins for large healthcare facilities.
RCM for Laboratories
Tailored solutions for labs to enhance coding accuracy, claims management, and financial operations.
Why Outsource Your Revenue Cycle Management to billingnavigator

Reduce Administrative Burden
Automate patient registration, eligibility verification, and claims processing—freeing your staff to focus on patient care.
Improve Cash Flow
Optimize reimbursement cycles and accelerate collections with accurate, timely claim submissions for steady cash flow.
Reduce Denial Rate
Identify and correct errors before submission to minimize claim denials, saving time and resources on rework and appeals.
Ensure Compliance
Stay compliant with payer requirements, coding standards, and regulatory guidelines to avoid penalties and legal risks.
Enhance Revenue Capture
Maximize reimbursements with complete documentation, precise coding, and thorough charge capture for all services rendered.
Gain Financial Insights
Access detailed reporting and analytics to track trends, monitor performance, and make informed revenue cycle decisions.
We Are Available Nationwide
Get your claims approved the first time! At BillingNavigator, our team consistently achieves a 95% first-pass clean claims rate. We identify and eliminate claim errors before submission, ensuring faster approvals and maximum reimbursements. Our proven process helps providers reduce rework, minimize denials, and maintain a smooth revenue cycle.
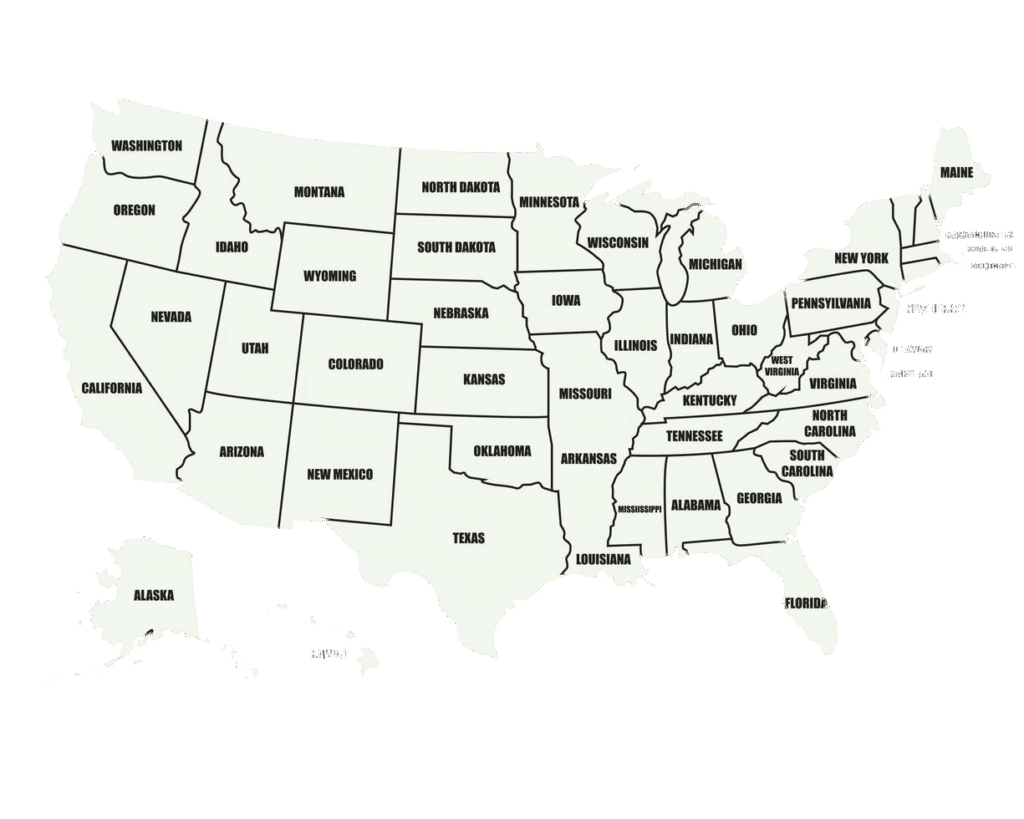
Schedule a Consultation
Around-the-Clock RCM Services for All Specialties
At BillingNavigator, we provide 24/7 revenue cycle management support across a wide range of medical specialties—from rheumatology and pulmonology to physical therapy and gastroenterology. Our RCM specialists understand the unique requirements of each specialty and are trained to navigate evolving healthcare regulations and reimbursement challenges. With tailored solutions and continuous support, we help your practice maximize revenue, reduce denials, and maintain financial stability at all times.
Cardiology
Gastroenterology
Oncology
OBGYN
Anesthesia
Neurology
Orthopedic
Radiology
Pediatric
Urology
Our Revenue Cycle Management Process & Workflow
Curious how BillingNavigator helps your practice achieve financial success? Our streamlined RCM workflow ensures every step of your revenue cycle is managed efficiently—from patient registration and eligibility verification to coding, claims submission, denial management, and payment reconciliation. With transparent reporting and continuous monitoring, our process maximizes reimbursements, reduces denials, and keeps your revenue flowing smoothly.
1. Patient Registration
Our process is initiated by collecting the relevant patient demographic information along with their insurance coverage details for proper registration.
2. Medical Coding
Our certified professional coders (CPCs) assign appropriate and accurate codes based on the rendered services and procedures.
3. Medical Billing
Based on the assigned codes in step 2, our billing specialists enter the service charges for rightful reimbursements.
4. Quality Review
Once the claim is ready, we perform a quality review in which our team checks the claims for coding inaccuracies and documentation inconsistencies.
5. Claim Submission
After ensuring the claim is error-free, we submit it electronically to receive the payment from the payer.
6. Payment Posting
Then comes the part where we record the payment collected from the relevant insurance company into the system.
7. Denial Management
In case a denial code is triggered, we thoroughly investigate it and file an appeal or rework the claim.
8. A/R Follow Up
A steady cash flow is a lifeline for any practice. We follow up with payers on unpaid and underpaid claims to ensure timely reimbursements.
9. Reporting
Finally, we generate detailed reports on your practice's financial performance to help you make data-driven decisions.
Competitive Pricing, Guaranteed
Looking for expert RCM support without straining your budget? BillingNavigator delivers affordable, tailored revenue cycle management solutions designed to meet the unique needs of your practice. We combine cost-effective services with expert workflow management to optimize reimbursements, reduce denials, and improve cash flow—helping you focus on patient care while we handle your revenue cycle efficiently.
The Importance of RCM Services for Healthcare Providers
Effective revenue cycle management is critical for optimizing your practice’s financial performance. BillingNavigator’s RCM services ensure accurate coding, efficient claims processing, timely A/R follow-up, denial management, and precise payment posting. By automating administrative tasks, we save your staff time and resources, reducing the need for claim rework and appeals.
Our RCM solutions also bridge the gap between providers, payers, and patients enhancing documentation, improving compliance with payer guidelines, and ensuring coders and billing specialists adhere to the unique requirements of each procedure. The result is faster reimbursements, reduced denials, and a more streamlined revenue cycle.

Connect with a Dedicated RCM Specialist
Partner with a BillingNavigator RCM specialist to streamline your practice’s revenue cycle operations. Our experts help maximize reimbursements, minimize denials, improve first-pass claim accuracy, and manage accounts receivable efficiently—so your staff can focus on delivering quality patient care while we optimize your financial performance.

FAQs
What is RCM in Healthcare?
Revenue Cycle Management (RCM) is the process that helps practices and hospitals obtain reimbursements for the care they provide. It begins with patient scheduling and registration and concludes with accurate payment reconciliation.
Does BillingNavigator offer RCM services for all healthcare specialties?
Yes. We provide tailored RCM solutions for every specialty, ensuring that your practice’s unique revenue cycle requirements are met efficiently.
Can BillingNavigator integrate with existing practice management systems?
Yes. Our team of trained RCM specialists ensures seamless integration with your current practice management and billing software, so your workflow remains uninterrupted while maximizing reimbursements.
Can BillingNavigator help improve cash flow?
Yes. By optimizing claim submissions, A/R follow-ups, and reimbursement cycles, we accelerate collections and maintain a steady cash flow for your practice.
Does BillingNavigator provide reporting and analytics?
Yes. We offer detailed, transparent reporting and revenue cycle analytics, helping practices make data-driven decisions and track financial performance.
Can BillingNavigator support small practices?
Absolutely. Our comprehensive RCM solutions serve solo practitioners, small and group practices, hospitals, and large healthcare systems, helping them optimize revenue and reduce administrative burden.
How much can I save by outsourcing RCM to BillingNavigator?
Outsourcing eliminates the need for costly infrastructure and an in-house billing team. You only pay a percentage of your monthly collections, making it a cost-effective solution. Contact our representatives for details on pricing.
How does BillingNavigator reduce claim denials?
We perform pre-submission claim scrubbing, identify errors, and ensure accurate coding and documentation to minimize denials and improve first-pass claim acceptance.
How does BillingNavigator ensure compliance?
Our team stays updated on payer rules, coding standards, and regulatory requirements. We train staff to ensure all claims comply with industry regulations, minimizing financial and legal risks.
Is BillingNavigator available for 24/7 support?
Yes. Our RCM specialists are available around the clock, ensuring continuous support for practices across all specialties.

